What Are the Different Types of Nursing Degrees?

Know before you read
At SNHU, we want to make sure you have the information you need to make decisions about your education and your future—no matter where you choose to go to school. That's why our informational articles may reference careers for which we do not offer academic programs, along with salary data for those careers. Cited projections do not guarantee actual salary or job growth.

Nurses continuously develop skills, clinical knowledge and expertise throughout their careers. Most people, though, think that “a nurse is a nurse is a nurse,” said Dr. Debra Murray, an adjunct instructor of nursing at Southern New Hampshire University (SNHU).
Murray spent 16 years serving in nursing roles in the U.S. Navy and holds a Doctorate of Nursing Practice. She received the Sentara Top Performing Provider Award in both 2017 and 2018, and she's a Certified Nurse Educator with additional certifications as a Public Health Clinical Nurse Specialist and pediatric primary care nurse practitioner.
“We have so many levels and paths toward practice, research and education," Murray said. “Nursing is a truly dynamic field.”
What Types of Nursing Degrees Are There?
Nurses can earn degrees at all different levels — from undergraduate programs to advanced options — to prepare them for many types of nursing specialties and focuses. While SNHU only offers bachelor's and master's degrees in nursing, there are nursing degrees at every educational level:
- Associate Degree in Nursing
- Bachelor of Science in Nursing
- Master of Science in Nursing
- Doctor of Nursing Practice
With each nursing degree level, you may have an opportunity to point your career in a direction that interests you.
And at SNHU, nursing programs are aligned with American Association of Colleges of Nursing (AACN) and Commission of Collegiate Nursing Education (CCNE) competencies and guidelines. They also feature new simulation technology for more hands-on experiential learning.
Find Your Program
Associate Degree in Nursing (ADN)
Note: Associate degrees in nursing are not currently available at SNHU.
Earning an associate degree in nursing is a great way to begin your nursing education and become a registered nurse (RN), even if you plan to level up in the future. Typically, associate degrees take two years to complete, meaning you could have an opportunity to take the National Council Licensure Examination (NCLEX) sooner.
 “That’s the licensing exam that deems a person competent to practice as an RN,” said Dr. Sonya Blevins, an adjunct instructor and a former director of compliance and licensure of nursing at SNHU. Like Murray, Blevins is a Doctor of Nursing Practice and Certified Nurse Educator. She also has over 20 years of teaching experience and is Certified Medical-Surgical Registered Nurse.
“That’s the licensing exam that deems a person competent to practice as an RN,” said Dr. Sonya Blevins, an adjunct instructor and a former director of compliance and licensure of nursing at SNHU. Like Murray, Blevins is a Doctor of Nursing Practice and Certified Nurse Educator. She also has over 20 years of teaching experience and is Certified Medical-Surgical Registered Nurse.
According to Blevins, once you've achieved licensure, you can begin practicing. When you're ready to earn your bachelor's degree in nursing, you can bring credits from your ADN to a transfer-friendly 4-year nursing school, like SNHU.
So, Can You Be an RN in Two Years?
The short answer is: yes. Most associate degrees take 18 months to three years to complete, and bachelor’s degrees typically take four years. How long it takes to become a nurse can vary depending on the degree level you choose. It’s also possible to accelerate the different types of degrees depending on your schedule and any transfer credits you may have.
After completing your degree, you must sit for the NCLEX exam and meet any additional state-specific requirements to attain the RN credential.
Read more about how long it takes to become a nurse.
Bachelor of Science in Nursing (BSN)
A BSN is a nursing focused bachelor's degree that's gaining importance throughout the field. In fact, 69.8% of surveyed nursing employers expressed a strong preference for candidates with a BSN, according to the AACN.
Some BSN programs can prepare you to become a registered nurse, while others, such as SNHU's, help you build on your existing experience.
The difference between an ADN and a BSN is the level of theory included in the curriculum. The associate degree can absolutely prepare you for a long and fulfilling career as a registered nurse. A BSN will also prepare you for a career as a nurse but adds the foundation that can ultimately allow you to pursue additional specialization and credentials.
RN to BSN degrees are intended for registered nurses who wish to advance their education. Your unencumbered RN license could count toward 45 credits at some schools with the opportunity to transfer even more credits from your associate degree, so you don’t have to start a four-year degree from scratch. At SNHU, for example, you could finish your BSN in as little as one year if you're already a registered nurse with an ADN.
Seeking a BSN program at an online university can give you the flexibility you need to progress your career and your education simultaneously. It may even enrich your experience, allowing you to apply what you're learning in the classroom to your day-to-day responsibilities as a nurse — and vice versa.
Learn more about if a BSN degree is worth it.
Is a BSN Higher Than an RN?
Not exactly. The ADN and BSN are degrees while an RN is a license. A degree alone is not enough to earn the designation of RN. Regardless of whether you choose to pursue an ADN or BSN first, you must also pass the licensing exam to become a nurse.
The BSN designation simply indicates that you have completed the 4-year degree program. The additional schooling in evidence-based practice, theory, research and management is covered in the education beyond the associate degree.
So, a BSN does indicate a higher level of schooling, but the exam to become and work as a registered nurse is the same for both credentials.

What Are Advanced Nursing Degrees?
The Master of Science in Nursing, or MSN, is available to those who wish to advance their education further. While MSN programs typically become available when a nurse earns their BSN, there are also accelerated programs you can find, such as an online RN to MSN pathway, to get you to the advanced degree faster.
SNHU students who participate in this pathway might see their programs reduced by six to nine credits — that's two to three courses fewer. If you participate in the HEaRT Challenge, you may have the ability to earn more courses or badges toward the accelerated MSN pathway, too.
If you're hoping to specialize in your career, an MSN program can give you the credential you may need. There are several focuses you can choose from when pursuing an MSN, such as:
- MSN in Family Nurse Practitioner (FNP) Degree (Note: SNHU's FNP degree is not available in all states)
- MSN in Healthcare Safety & Quality Degree
- MSN in Nursing Education Degree
As technology is increasingly integrated into the practice of medicine, the nursing profession is evolving to include specialties to support that. “Nursing informatics is a new and interesting specialty,” said Blevins. “This sub-specialty came out of the need for all hospitals to have electronic medical documentation. With this degree, you’ll be able to collaborate with the technology side to implement changes and new technologies."
Another popular career role for nurses obtaining an advanced degree is a nurse practitioner. A nurse practitioner is a healthcare provider that comes from a nursing background. There are many levels of specialty within being a nurse practitioner, including:
- Acute care
- Gerontology
- Mental health
- Pediatrics
- Primary-based
 Nursing education degrees allow nurses to teach in academic or hospital settings. This field focuses on maintaining regulatory requirements, patient safety and quality, and making hospital healthcare, in general, safer for the patient.
Nursing education degrees allow nurses to teach in academic or hospital settings. This field focuses on maintaining regulatory requirements, patient safety and quality, and making hospital healthcare, in general, safer for the patient.
"Nursing education was my calling, my meant-to-be," said Cheryl Marcotte '23MSN.
Marcotte earned her MSN in Nursing Education from SNHU. "I am privileged to have just recently been offered a full-time academic faculty position and the possibilities are now a reality," she said.
What is the Highest Nursing Degree?
There are also several types of terminal degrees available to nurses. Terminal degrees indicate that you have reached the highest level of education in your field.
Three types include:
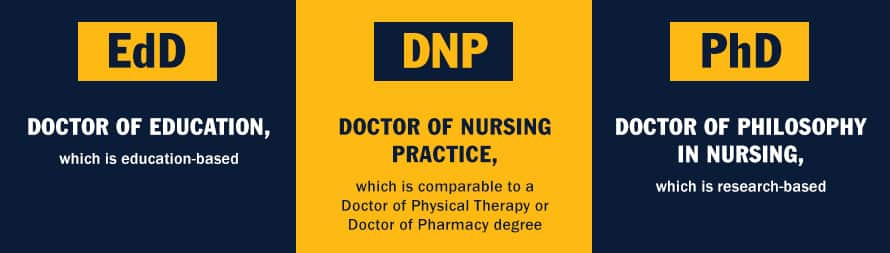
Note: SNHU does not currently offer doctorate degrees in nursing.
While a terminal degree is certainly not necessary to have a long and rewarding nursing career, the additional credential will provide even more options in a field that is already very customizable.
Blevins decided to earn her Doctor of Nursing Practicing (DNP) after a successful career spent working in obstetrics, cardiac critical care and medical-surgical nursing. She went back to school for the credential because of the additional opportunities and flexibility it provided to her career.
“For me, personally,” she said, “the DNP has allowed me growth and opportunity with my career as well as the flexibility to take a remote position with SNHU and continue my career with a focus on nursing education.”
What is the Hardest Nursing Specialty?
All areas of nursing can be challenging, and all can be rewarding. “Every nursing specialty has its pros and cons,” said Blevins. “For example, with labor and delivery, if you have an unstable mom or a baby in distress, that is very challenging."
Of course, any specialty will have its challenges when it comes to the need to comfort families as well as care for patients. The other side of that, though, is that the pros are meaningful.
“You are able to really help people, right at their bedside,” said Blevins. “Everything from helping a patient improve to helping students become nurses and helping them grow professionally while being a source of support. These are the wonderful parts of nursing.”
What Kind of Nurses Get Paid the Most?
![]() Certified Registered Nurse Anesthetists (CRNAs) make the highest salary, according to Murray.* In 2023, nurse anesthetists earned a median salary of $212,650, the U.S. Bureau of Labor Statistics (BLS) reported.* BLS noted that this career path typically requires at least one year working as an RN in a critical care setting and additional education. (Nurse anesthesia programs are not currently offered at SNHU.)
Certified Registered Nurse Anesthetists (CRNAs) make the highest salary, according to Murray.* In 2023, nurse anesthetists earned a median salary of $212,650, the U.S. Bureau of Labor Statistics (BLS) reported.* BLS noted that this career path typically requires at least one year working as an RN in a critical care setting and additional education. (Nurse anesthesia programs are not currently offered at SNHU.)
Aside from CRNAs, Blevins said those in leadership positions typically earn higher salaries than other nurses.* For example, BLS said medical health and service managers made a median of $110,680 in 2023.*
"It all depends on the setting and level of training and experience that you have,” Blevins said.
The typical median salary for registered nurses as of 2023 was $86,070 per year, according to BLS, which is significantly higher than the median national average for all careers.* There's faster than average projected growth in nursing, too, with a predicted 6% increase through 2033, BLS reports.*
BLS said nurses in hospitals earned median salaries of $88,430 in 2023 because their work involves round-the-clock and critical care.* Nurses in ambulatory healthcare services see patients for routine medical care outside of a hospital setting, and they earned a median salary of $81,230 in 2023, BLS reported.* And nurses who provide care in nursing and residential care facilities earned a median salary of $79,280 in 2023, according to BLS.*
While working in an educational setting commands a lower salary than bedside or ambulatory nurses, with a national median of $71,550 per year, nurses working in education still earned above the national median, BLS notes.*
If you earn a specialized advanced degree, your potential earnings could increase. For example, BLS reports that nurse practitioners earned $126,260 in 2023.*
Careers at Every Level
If you’re not sure which specialty is right for you, don’t worry. Nursing is flexible.
You don’t have to declare a specialty at first. “You will learn very quickly through clinical experiences what you like and don’t like,” said Blevins. “A good nursing program (can) help you figure out your path by the time you graduate,” she said.
“One unique thing about nursing is that you truly can work your way through the system," said Murray. "You can start as a medical assistant, then LPN, then RN, and on to graduate school if you wish, all while working and earning a living plus gaining valuable experience."
Ultimately, the nursing profession can offer many employment prospects, ways to customize your career and the potential to gain valuable professional experience — all while you work your way through school. And perhaps the best part of the nursing profession is the many opportunities to make a real difference in the lives of others.
A degree can change your life. Find the SNHU online nursing program that can best help you meet your career goals.
*Cited job growth projections may not reflect local and/or short-term economic or job conditions and do not guarantee actual job growth. Actual salaries and/or earning potential may be the result of a combination of factors including, but not limited to: years of experience, industry of employment, geographic location, and worker skill.
A former higher education administrator, Dr. Marie Morganelli is a career educator and writer. She has taught and tutored composition, literature, and writing at all levels from middle school through graduate school. With two graduate degrees in English language and literature, her focus — whether teaching or writing — is in helping to raise the voices of others through the power of storytelling. Connect with her on LinkedIn.
Explore more content like this article

Academic Spotlight: Dr. Shakera Moreland, Health Sciences Clinical Faculty Member

SNHU Hosts 5th Annual Global Summit for Healthcare Professionals

How to Become a Nurse in 4 Steps
About Southern New Hampshire University

SNHU is a nonprofit, accredited university with a mission to make high-quality education more accessible and affordable for everyone.
Founded in 1932, and online since 1995, we’ve helped countless students reach their goals with flexible, career-focused programs. Our 300-acre campus in Manchester, NH is home to over 3,000 students, and we serve over 135,000 students online. Visit our about SNHU page to learn more about our mission, accreditations, leadership team, national recognitions and awards.


